Blur, loss of contrast sensitivity, light sensitivity, glare, visual field loss, distortion, nystagmus, color vision anomalies, and double vision are types of vision loss. Each of these disorders can cause decreased vision independently, however, there is frequently more than one factor that contributes to vision impairment.
Click to see video for “Types of “Vision Loss”:
Understanding the Different Types of Vision Loss
Vision loss encompasses a wide range of challenges, from blurriness and sensitivity to light, to more complex issues like distortion and color vision anomalies. These conditions not only affect how clearly we see but also impact our daily lives in various ways.
What is visual acuity?
Acuity is the ability to see fine lines and forms as measured by the visual acuity charts used by your eye doctor.
Exploring Visual Function: Beyond Visual Acuity
More nuanced than visual acuity is the concept of visual function. Visual function is not as straightforward to measure. It’s intriguing that an individual may possess good measured visual acuity, yet encounter difficulties using their eyes in real-life scenarios where lighting is inadequate, or contrast is lacking. On the other hand, someone with very poor measured visual acuity might possess remarkable adaptive visual abilities, allowing them to function effectively despite their impairment.
Visual function goes beyond just the clarity of vision. It encompasses the ability to navigate the complexities of the visual world, from adapting to varying light conditions to discerning objects in low contrast environments.
Types of Vision Loss
Blur
One of the most recognizable forms of vision loss is blur. It describes an area of unclear vision where lines and details appear fuzzy and lack sharpness. This blurring can lead to a reduction in both visual acuity and visual function. Blur can be broadly defined as an overall haziness or specifically as an area of indistinct vision.
When blur affects the central area of the eye, known as the macula, it can significantly impair visual acuity. Conversely, if the blur occurs in the periphery of the eye, its impact on visual acuity is typically less severe. Let’s delve deeper into the nuances of blur and its effects on our ability to see clearly.
Adaptive Strategies: Individuals with chronic blur often develop adaptive strategies. These might include using magnifiers for reading, increasing lighting in their environment, or relying more on other senses to compensate for reduced visual clarity.
Clear image and generalized blur.


Loss of Contrast Sensitivity
Contrast is the key factor that allows objects to stand out from their backgrounds. It refers to the difference in the amount of light reflected from objects compared to their surroundings. The ability of our visual system to detect this difference is known as contrast sensitivity.
Contrast sensitivity is a subtle aspect of our visual function that can be challenging to describe and measure accurately.
During an eye examination, an eye doctor typically measures visual acuity using a chart with high-contrast black letters against a white background, as this provides the highest level of contrast.
The higher your contrast sensitivity, the less light you need to see objects clearly. Conversely, reduced contrast sensitivity can significantly impact visual function. It can lead to difficulties in adapting to changes in light levels and navigating dimly lit environments.
Situations with low contrast, such as dimly lit rooms or reading materials with subtle contrasts like grey print on yellowish paper, pose challenges for individuals with diminished contrast sensitivity. These conditions can make it challenging to read newspapers or decipher printed materials with colored text on colored backgrounds.
Adaptive Strategies. Those who have problems with contrast sensitivity should use optimal lighting, high contrast materials, filters for eyeglasses, illuminated magnifying devices. and environmental modifications such as texture and tactile cues.
High contrast and Low contrast.


Light Sensitivity and Glare
The optimal light levels for visual performance vary depending on the individual’s eye condition and preferences. While some visual conditions benefit from increased light levels, others can lead to heightened light sensitivity, making bright lights or sunshine uncomfortable.
Due to the way light-sensitive neurons in our visual system are wired, individuals with retinal diseases often find bright lights exceedingly intense and challenging to adapt to, leading to light sensitivity, also known as photophobia. Conditions such as Stargardt’s disease, achromatopsia, or albinism can make increasing light levels uncomfortable for those affected.
Glare is another factor that contributes to light sensitivity and loss of contrast sensitivity. People with vision impairments may struggle with high light levels due to glare, which can originate from external sources or within the eye itself.
Glare occurs when a light source or reflective object is bright enough to overpower the ability to see surrounding objects clearly. Even the average person can experience glare from reflective surfaces, like water, or when driving into the late afternoon sun. However, for individuals with light sensitivity, external glare can be particularly bothersome and disabling.
Adaptive strategies. Those with light sensitivity and glare with visual impairments should take proactive measures to manage their environment and enhance their comfort and safety. From adjusting lighting conditions to wearing specialized eyewear, there are various strategies available to mitigate the effects of light sensitivity and glare.
Bright , clear image . Brightness overpowers visible details.


The other way glare can impact vision is by internal reflections within the visual system. Light entering a normal healthy eye has a clear path through the eye to the light-sensing cells at the back of the eye. Any process that infringes on the clarity of the parts of the eye can cause scatter, meaning the light will not be crisply focused to the back of the eye, but will instead bounce around, creating the phenomenon of internal glare. Damage to the cornea, lens cataracts, and vitreous floaters can contribute to internal glare.
Bright sharp details . Details obscured by glare.


Visual Field Loss and Scotomas
The visual field encompasses our entire area of vision, including the central macula and the peripheral visual areas. Our visual fields from both eyes overlap, providing us with a panoramic view of the world, spanning approximately 190 degrees horizontally for those with normal binocular vision. While our peripheral vision is not as detail-sensitive as the central macular area, it plays a crucial role in detecting light and motion, aiding in our orientation and mobility.
Loss of central vision results in diminished visual acuity, affecting tasks like reading and facial recognition. The loss of peripheral vision impacts our ability to navigate and orient ourselves efficiently in our surroundings.
Scotomas are blind spots or areas of depressed vision that occur due to retinal cell death. Their impact depends on factors such as location, size, depth, and whether they affect one eye or both.
Central scotomas, particularly devastating to visual acuity, affect the central macular area rich in densely packed light-sensitive neurons (cones). Conditions like age-related macular degeneration and Stargardt’s disease target this area, leading to difficulties with reading and recognizing faces. Despite reduced visual acuity, individuals with central vision loss can often maintain functional vision by utilizing their peripheral vision and learning techniques like eccentric viewing.
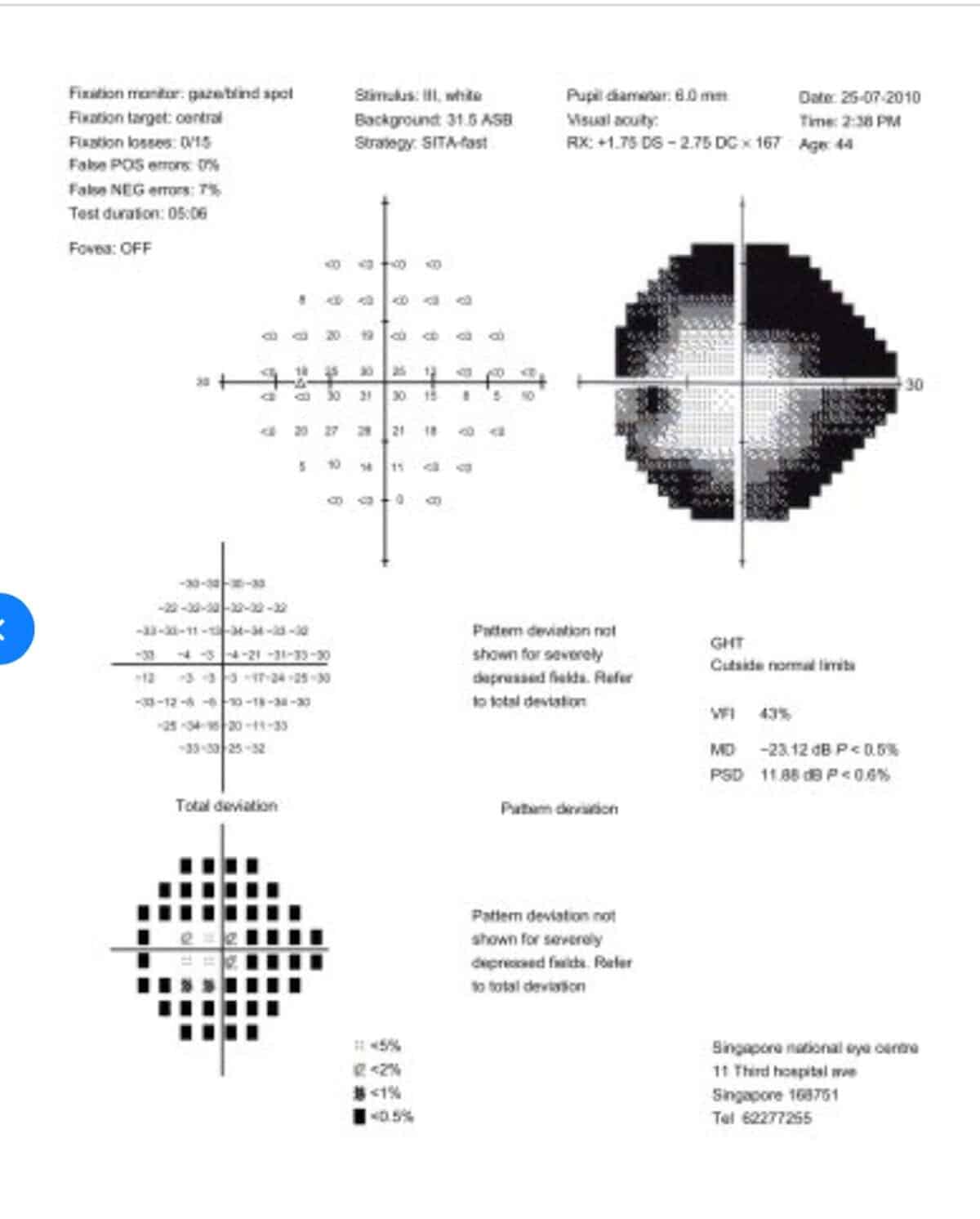
Peripheral field loss refers to areas outside the macula, affecting the rest of the retina. This loss can manifest as sections, entire hemispheres, or localized areas. Diseases such as glaucoma and optic neuritis can lead to significant peripheral visual field loss.
Central vision loss, comparable to how those with macular degeneration see.

Peripheral field loss refers to areas outside the macula, affecting the rest of the retina. This loss can manifest as sections, entire hemispheres, or localized areas.
Diseases such as glaucoma and optic neuritis can lead to significant peripheral visual field loss.
Peripheral field loss . Humphrey visual field analysis.


A significant area of vision loss can profoundly impact daily functioning. Blind spots or large areas of visual impairment can create challenges in navigation, increasing the risk of collisions with objects or architecture not seen in the visual field.
Retinitis pigmentosa stands out as one of the most striking diseases causing visual field loss. This degenerative condition can affect substantial portions of the retina, sometimes leading to the complete loss of the peripheral visual field. In such cases, the remaining field of vision shrinks to a mere 10 to 20 degrees, severely limiting the individual’s ability to perceive objects and surroundings.
Distortion
Visual distortion is a common phenomenon that often occurs in the central vision area known as the macula, but it can also manifest anywhere in the visual field. To illustrate, imagine the light-sensitive photoreceptor cells in the retina standing upright like soldiers, neatly arranged elbow to elbow in orderly rows. However, if fluids or waste toxins disrupt this orderly arrangement, the photoreceptors become disarrayed.
The brain perceives this disarray as visual distortion. For example, lines on the road may appear wavy instead of straight, the edges of walls might seem to tilt, and letters in words may appear jumbled or distorted. This distortion can vary in intensity and can greatly impact daily activities such as reading, driving, or recognizing faces. Understanding the underlying causes of visual distortion is crucial for individuals experiencing these symptoms, as it can lead to appropriate management and treatment strategies.
Exaggerated central vision distortion.

Nystagmus
Nystagmus is a condition characterized by rhythmic, involuntary movements of the eyes, leading to decreased vision. This movement can cause the eyes to appear to ‘jiggle,’ and the term used for this phenomenon is oscillopsia. As a result of this constant movement, it becomes challenging for the eyes to fixate and observe details, resulting in blurred vision.
The direction of nystagmus movement can vary, including side to side, up and down, or even in a circular motion. Additionally, the magnitude of movement can differ in terms of size, speed, and frequency. These variables can be further influenced and exacerbated by factors such as fatigue, excitement, or stress.
Management strategies often focus on improving visual function and reducing the impact of the eye movements on visual clarity.
Clear stable image, blur due to the eye movement of nystagmus


Color Vision Anomalies
Color deficiencies can occur as either congenital anomalies or acquired conditions due to disease processes.
The term “color blind” is often used to describe a common congenital color deficiency that affects 8 to 10 percent of the population, predominantly males. This form of color vision anomaly is more accurately termed as a color deficiency or partial color vision. It’s not that individuals with color deficiency don’t see color; rather, they lack the photopigment sensitivity to certain wavelengths of light.
The most common type of color deficiency affects the red-green wavelengths, causing red and green hues to appear similar and be easily confused. A rarer anomaly affects the blue-yellow range. Congenital color anomalies affect both eyes equally and are stable, meaning they do not worsen over time and are not part of a disease process.
Achromatopsia, also known as rod monochromacy, is another type of congenital color anomaly. This condition involves a deficiency in all three photopigments: red, green, and blue. The severity of achromatopsia can vary, with the most extreme form resulting in complete color blindness. Individuals with achromatopsia often experience extreme light sensitivity, reduced visual acuity, and nystagmus.
Acquired color deficiencies occur after birth and are associated with disease processes. Unlike congenital deficiencies, acquired deficiencies may affect one eye more than the other and are not stable. Changes in color sensitivity are often accompanied by a decrease in visual acuity.
Hereditary eye diseases such as Best’s Vitelliform Dystrophy, Stargardt’s Disease (juvenile macular degeneration), and retinitis pigmentosa can lead to changes in color sensitivity as the disease progresses.
Adult-onset diseases like diabetes, glaucoma, and cataracts can also impact color vision. Notably, cataracts act as a yellow filter that can influence color perception.
Optic nerve diseases such as optic atrophy or optic neuritis can affect color perception as well. Optic neuritis, characterized by inflammation of the optic nerve and its myelin sheath, results in decreased visual acuity and colors appearing pale and washed out. This condition can be associated with multiple sclerosis, autoimmune diseases, and infections.
Optic nerve atrophy is a process where the nerves of the optic nerve begin to die, leading to decreased visual acuity, scotomas, visual field loss, and loss of color perception. Conditions that affect blood flow to the eye and optic nerve, such as strokes, hypertension, exposure to toxins (like alcohol abuse), and trauma, can also result in optic nerve atrophy.
Double Vision
Double vision, known as diplopia, can manifest in two forms: monocular or binocular.
Monocular diplopia occurs when two images are seen with just one eye open. To test for monocular double vision, cover each eye separately. If the doubling persists with only one eye open, it is likely monocular. Causes of monocular double vision range from common issues like uncorrected astigmatism, which can be corrected with eyeglasses, to more serious conditions such as corneal disruption from keratoconus, corneal scarring, lens disruption like cataracts, or traumatic injury.
Binocular double vision occurs when both eyes are open, and the images from each eye are not properly aligned. In normal vision, the images from both eyes are fused. This fusion is achieved through the ‘yoking’ of nerves and muscles during the development of the visual system before birth. It’s akin to a team of oxen with a yoke, moving together in the same direction at the same speed. This yoking ensures that the eyes move and fixate on objects together, maintaining a single, unified image.
Any process that damages or disrupts these yoked nerves or muscles can lead to binocular double vision. Double vision can occur due to disturbances along the visual pathway of the optic nerve or within the visual cortex of the brain, resulting in misaligned images. This misalignment can manifest as side-by-side, up-and-down, or tilted images.
The spacing between the two images may vary, appearing widely separated or as a slight ghosting of overlapping images. Double vision may be transient, occurring briefly and intermittently, or it may be episodic, with resolution dependent on the underlying disease course, or even permanent.
Various neurological and neuromuscular disorders can cause binocular double vision. Conditions such as myasthenia gravis affect nerve and muscle function, potentially leading to partial or full paralysis (paresis) of the eye muscles. Vascular diseases like diabetes and high blood pressure, as well as vascular events such as strokes, can also impact nerve and muscle function in the eyes.
Space-occupying lesions such as tumors or pituitary adenomas can affect nerve and muscle function, leading to double vision.
Trauma to the head, face, or orbital cavity can result in nerve damage or the entrapment and damage of eye muscles, causing diplopia.
Individuals experiencing double vision should seek evaluation from an eye care professional to determine the underlying cause and appropriate treatment options.
Interested in other visual phenomena? See: Vision Loss and Visual Disturbances: Phenomena that may be experiencd by those with low vision
or
Understand how vision loss may affect your life: How Vision Loss Affects the Social, Emotional, and Practical Aspects of Life
In the End…
Vision impairment is a complex and multi-faceted challenge. It extends beyond mere loss of visual acuity to include a combination of various factors that contribute to an overall decline in visual function.
Understanding these factors and their interplay is crucial in developing comprehensive strategies to manage and improve visual capabilities. Whether it’s addressing blur, contrast sensitivity, visual field loss, color vision anomalies, or double vision, each aspect requires careful consideration and tailored approaches. By recognizing the nuances of different types of vision loss, individuals and healthcare professionals can work together to enhance visual function and quality of life for those affected by these conditions.

