Your risk for AMD increases with age, but it is not inevitable or blinding. It is not curable, but can be prevented. Life is not over with a diagnosis of AMD, there are some treatments available.
Truth #1 The risk for developing macular degeneration increases with age.
Population studies have consistently demonstrated a correlation between visual acuity and age, revealing a higher prevalence of vision impairment and legal blindness as individuals grow older. This trend is most pronounced among those aged 65 and above, with a notable escalation in incidence beyond the age of 75.
According to data from the Centers for Disease Control and Prevention (CDC), an estimated 2.95 million Americans aged 40 and above are affected by age-related macular degeneration (AMD), a figure that rises to 67 million across the European Union. AMD stands as the primary cause of permanent vision impairments among individuals over 65, with a particularly elevated occurrence among those of European descent.
The World Health Organization (WHO) approximates that the United States witnesses 200,000 new cases of AMD annually, while Europe experiences 400,000 new cases per year. Projections from the WHO indicate a global population of 196 million individuals with AMD in 2020, with an anticipated increase of 100 million cases by 2040, bringing the total to 288 million cases worldwide.
With our population aging, there is a proportional rise in the percentage of older age cohorts. Consequently, research indicates a forthcoming surge in the number of individuals grappling with vision impairments. Addressing these challenges falls within the purview of low vision rehabilitation, a specialized field within vision care.
Truth #2 Macular degeneration is not inevitable as we age.
The progression of vision loss associated with aging, such as macular degeneration, is not an inevitable fate. While maintaining good vision as we age is indeed achievable, numerous factors come into play that can influence the health of our eyes and overall well-being. Macular degeneration, in particular, is a complex condition influenced by various factors including general health, genetics, and environmental elements.
Research has underscored the connection between eyesight and overall health, highlighting the crucial role of nutrition in maintaining optimal eye health. Certain nutritional components found in our diet have been identified as essential for supporting eye health, with evidence suggesting that specific supplements may even slow down or reverse the degenerative process.
Furthermore, studies have elucidated the interplay between genetics and environmental factors. Our genes, comprising intricate code sequences within our genetic material (DNA), interact with external influences to determine gene expression. External factors like UV light exposure, medication use, and dietary toxins can impact gene activity, thereby influencing the development of degenerative eye conditions such as macular degeneration, glaucoma, or cataracts.
Regular exercise is also fundamental to promoting overall health, as it enhances blood vessel flexibility and circulation. This ensures adequate oxygenation and nutrient delivery to the delicate blood vessels of the eye, supporting their optimal function.
Moreover, prioritizing routine eye examinations is paramount. Early detection of eye diseases, coupled with expert guidance from a responsive eye care professional, can significantly impact the prognosis of these conditions.
Ultimately, the choices we make regarding diet and lifestyle significantly influence how we age. By adopting a proactive approach to eye health through proper nutrition, exercise, and regular check-ups, we empower ourselves to maintain optimal vision and overall well-being as we navigate the aging process.
Truth #3 It is not inevitable that those with macular degeneration will go blind.
Macular degeneration, while often associated with severe vision impairment, does not invariably lead to complete blindness. However, the classification of blindness can vary depending on the criteria applied.
Is macular degeneration considered legally blind?
The American Medical Association initially outlined a definition of blindness, which was subsequently adopted by entities such as the Social Security Administration for eligibility determinations and by the legal system as a standard definition. Many individuals affected by AMD receive state and government assistance due to their legal designation as blind.
According to the criteria established by these agencies, legal blindness is defined as having visual acuity no better than 20/200 (6/60) in the better eye, even with the best prescription for eyeglasses or contact lenses. It’s important to note that being legally blind does not imply total vision loss or the absence of functional vision.
Consider the nature of age-related macular degeneration: It entails the progressive degeneration of the central area of vision known as the macula, leading to diminished visual acuity.
Our ability to perceive visual acuity relies on the densely packed sensory neurons in the central vision area. This region, characterized by a high concentration of neurons, is particularly susceptible to fluctuations in oxygen and nutrient levels. Consequently, it is the central area of acute vision that is most profoundly affected by various health and environmental factors.
The Stages of Macular Degeneration.
There are stages to ‘dry’ macular degeneration. It is only the final advanced stages that results in “legal blindness.’ 90% of those diagnosed with macular degeneration have the dry form. 10% go on to the vision devastating ‘wet’ form of macular degeneration.
Early ‘Dry macular degeneration:

- Developed slowly,
- characterized by white small deposits called drusen,
- causes some visual acuity loss: 20/20 to 20/40 (6/6 to6/12).
Intermediate ‘dry’ macular degeneration:
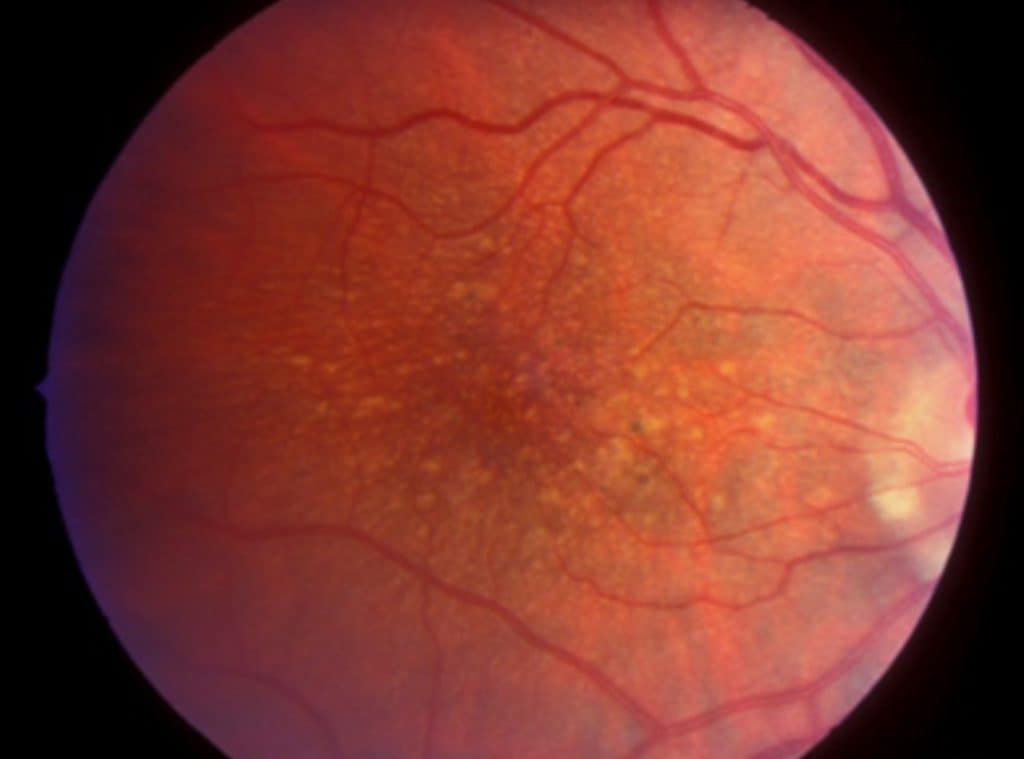
- Slow, progression continues,
- accumulation of more and larger drusen,
- more visual acuity loss; 20/40 to 20/100 ( 6/12 to 6/30).
,

Atrophic ‘dry’ macular degeneration;
- End stage of ‘dry’ macular degeneration,
- death of the retinal cells of the macula,
- visual acuity, less than 20/200 (6/60), ‘legally blind.’
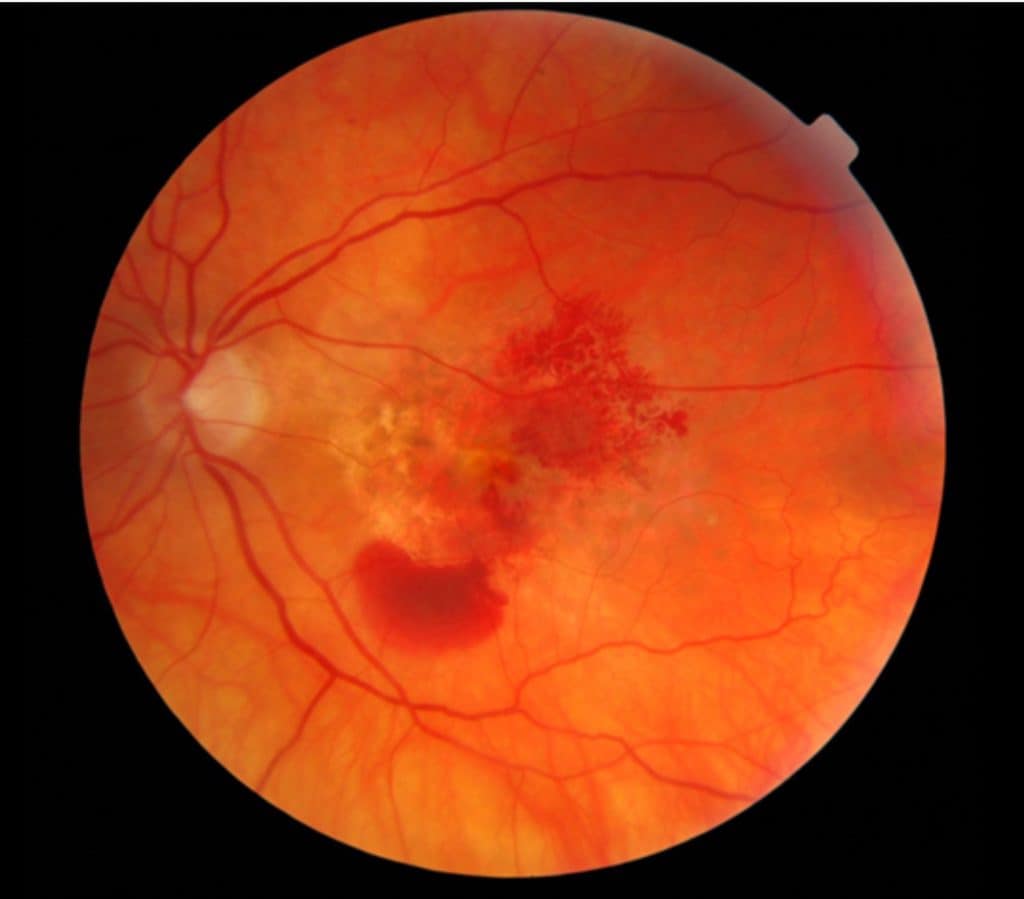
‘Wet’ macular degeneration;
- A sudden, rapid loss of central vision,
- inflammatory process, characterized by leakage and bleeding of blood vessels beneath the macula, resulting in scarring.
- Most severe devastating loss of vision, visual acuity, less than 20/200 (6/60).
Can You still see with MD?
Commonly, MD is often linked with the perception of older individuals losing their sight. However, the reality is that significant residual vision typically persists.
While the macula may be affected, the remainder of the retina remains functional. Vision continues to operate in these peripheral regions. Admittedly, visual acuity may not be as precise as in the macula due to the lower concentration of nerve endings in these areas.
The crucial aspect lies in learning to utilize these surrounding areas of the macula through techniques such as eccentric fixation, also referred to as eccentric viewing or ‘preferred retinal locus.’
Truth# 4 There is no cure for macular degeneration.
Just as there is no cure for the bodily changes associated with aging, there remains no definitive cure for age-related macular degeneration (AMD). While the cells throughout our body possess remarkable capabilities for replication throughout our lives, the same cannot be said for the cells of the retina.
The retinal epithelial cells (RPE) play vital roles in sustaining the retina and the underlying blood vessel layer. However, the RPE possesses a limited capacity for division before ceasing to function. With age, both the number and function of these cells decline. Ideally, they should persist throughout our lifetime unless subjected to factors such as oxygen deprivation, poor diet, excessive UV light exposure, and other sources of oxidative stress, compounded by genetic predispositions.
As RPE cells begin to perish, waste products from retinal metabolism accumulate as drusen. Consequently, the deterioration of retinal cells and RPE leads to impaired vision, and currently, there exists no effective means to restore them.
Nevertheless, while a definitive cure remains elusive, there are treatments and preventive measures available for managing AMD and potentially slowing its progression.
Truth #5. There are treatments available.
As you peruse the internet, you’ll encounter numerous articles addressing treatments for the ‘wet’ form of AMD. However, I’d like to first delve into the more prevalent form known as ‘dry’ AMD.
Currently, there exists no medical remedy for ‘dry’ macular degeneration, largely due to its multifaceted nature, wherein genetics, general health, and environmental factors intertwine.
Here’s what researchers are investigating:
Oxidative stress plays a pivotal role in the onset and progression of degenerative diseases, particularly in the eye given its intricate structure and function.
Oxidative stress is a metabolic process leading to cellular and tissue damage, spurred by byproducts of oxygen metabolism, UV radiation, pollutants, and heavy metals. These byproducts, known as free radicals or reactive oxygen species (ROS), are typically produced as part of normal metabolic processes. However, when they accumulate with age, they become detrimental to cells and tissues.
Evidence suggests a correlation between oxidative stress and AMD. Consequently, researchers, physicians, and patients are exploring avenues to counteract free radicals, notably through antioxidants.
Fruits and vegetables stand out as excellent sources of natural antioxidants. Studies have revealed an inverse relationship between diets rich in natural antioxidants and the prevalence of AMD. In other words, higher antioxidant intake is associated with lower AMD risk.
Additionally, research has shown that supplementation with antioxidants enhances resistance to AMD.
Best supplement for Eyes? Read; What is the Best Supplement to Preserve Eye And Brain Health?
Probably the most commercially successful study was the Age Related Eye Disease Study (AREDS). This study demonstrated that daily supplementation with a formula of antioxidants, slowed the progression of intermediate to advanced AND by about 25%.
Description of the ARED study: How do the AREDS and AREDS 2 Differ?
Can you stop the progression or reverse macular degeneration?
The best you can hope for is to halt or slow the progression of ‘dry’ AMD. The best weapon available is diet and supplementation with anti-oxidants.
The first thing to do is to adjust your diet to include a variety of healthful, whole foods namely fruits and vegetables. These should be prominent in your diet. To ensure adequate amounts of anti-oxidants, the minimum supplements to take are:
Vitamin C Studies have shown that Vitamin C is found in high levels in the eye, and has an effect of preventing free radical formation from UV light. Take 2000 – 3000 mg / day.
Vitamin E Also protects against free radical damage from UV light exposure and maintains integrity of the lipid membranes of cells. Dosage; 400 IU /day
Carotenoids, especially lutein and zeaxanthin. The macula has the highest concentration of these two carotenoids in the body, They have a vital function supporting cell function and scavenging ROS. Dosage: lutein 10 mg /day zeaxanthin 2 mg /day.
This is the minimum. A diet and supplementation regiment high in vitamins and minerals is necessary to maintain good physical and eye health. You might be interested in this other article: ‘3 Most Commonly Recommended Eye Supplements.’
Treatment of ‘Wet’ AMD
10% of those with ‘dry AMD, go on to ‘wet’ AMD. Although only 1o% develop the ”wet ‘form, it is responsible for 85% of those who are legally blind from AMD.
This disease is most commonly found in those with vascular disease.
The complicating factor is the growth of abnormal blood vessels underneath the macula. This growth of new, abnormal blood vessels is called neovascularization. These blood vessels grow in response to low oxygen levels in the retina. The fragile blood vessels are susceptible to breakage and leakage, which results in more fluid and blood in the macula. These pockets of fluid and/or blood are damaging and toxic to the vital cells that support the macula.
Treatments
The treatment for the’ wet’ form of ARMD requires timely detection and intervention by the eye doctor. Timely detection of macular changes is usually done by self monitoring. Here is an article on “Monitoring for the Progression of AMD.‘ Treatment during the early stages, although it will not reverse damage already done to the central vision area, can reduce the severity of vision loss. There are three techniques to halt the growth of abnormal blood vessels, thereby limiting potential damage:
1. Injection Only. Injection into the eye of a drug that stops the development of new, weak and fragile blood vessels. The drug is called anti-VEGF. VEGF (vascular endothelial growth factor) is produced by the oxygen starved tissues of the eye to promote the abnormal blood vessel growth. Although growing new blood vessels seems like a good idea, these new blood vessels are problematic in that they are fragile. The anti-VEGF drug injection stops the growth to alleviate the problem. (Drug names: Avastin, Lucentis, Eylea, Beovu)
The injected drug is effective for 1 to 2 months, therefore repeat injections are needed every 4 to 8 weeks. Thus far, anti-VEGF injections have been successful in slowing AMD progression and in some cases, there has even been improvements in vision.
2. Injection and Laser. The drug (Visudyne®) is injected into the arm and within minutes is taken up by the fragile new vessels of the macula. The injection is followed by a laser treatment to the affected area of the eye to activate the drug. The drug then closes off the abnormal blood vessels to stop the growth and subsequent leaking and bleeding. This is called photodynamic therapy. This treatment is not permanent, and may need to be repeated in three months.
3. Laser Only. Laser treatment is done around the area of the macula that in effect, destroys the surrounding leaky blood vessels. It is not likely to be done in the macular area, as it can destroy the sensitive retinal cells above the targeted blood vessels, leaving a little blind spot. This is called photocoagulation laser therapy.
All three of these treatments are done in the retina specialist’s office on an outpatient basis.
Before you get to this stage, learn how to prevent AMD.
Truth #6 MD is preventable.
Age related Macular degeneration occurs after a lifetime of use and possibly abuse. The truth for those that have been diagnosed with AMD is that it does not have to progress.
1. Healthy body, healthy eyes.
Macular degeneration often arises from a body that has other health issues. Hypertension, nutrient deficiency (poor diet and poor digestion), cardiovascular disease, and diabetes have all been implicated as risk factors. Stricter attention to diet and monitoring and care of other health concerns can reduce the risk of development and progression of eye disease.
High blood pressure medications can have the effect of depleting water soluble vitamins and minerals. So consider supplementation with high blood pressure medications.
2. Healthful diet and supplement the rest
Eat a diet high in fruits and vegetables. Try to incorporate fatty fish (for the fish oils). If you can’t eat fish, consider supplementing with the omega 3’s (DHA and EPA)or flaxseed oil.
Avoid vegetable oils that are processed, like basic vegetable oil, and corn oil (Olive oil and avocado oil are cold pressed and unrefined. Those are OK.) Also, avoid processed foods, many contain mono- and polyunsaturated oils. Avoid high sugar and white flour consumption, both of which are low in nutrients and high in calories.
Think heart healthy diet; Good not only for the heart, but good for the eyes as well.
3. Stop Smoking.
The chemicals introduced to the body through smoking are toxic to the blood vessels and retina. Studies have shown that smoking can double the risk for AMD. (click for article: JAMA Ophthalmology)
4. Wear UV protective sun wear
A lifetime of chronic UV and blue visible light exposure is thought to be one of the causes of age-related macular degeneration. The normal eye, when subjected to intense or chronic UV radiation exposure can suffer photo-chemical changes to its tissues. A diseased eye may be even more susceptible to UV and ‘near’ UV’ damage. UVA and UVB pass through the atmosphere, even through a cloud cover, and can have a negative effect on our skin and eyes.
5. Get Regular exercise.
The health benefits of regular exercise to prevent weight gain and degenerative disease is well publicized. Exercise lowers the risk for cardiovascular disease and improves cognitive function. Both of these benefits are relative to eye heath.
The increased blood flow to the eyes during exercise and after, provides oxygen and nutrients to the retina and supporting structures.
The American Heart Association recommends;
- Get at least 150 minutes per week of moderate-intensity aerobic activity or 75 minutes per week of vigorous aerobic activity, or a combination of both, preferably spread throughout the week.
- Add moderate- to high-intensity muscle-strengthening activity (such as resistance or weights) on at least 2 days per week.
See their full recommendations here: heart.org
6. Know your risk factors.
The most significant of these are:
- age
- positive family history
- cigarette smoking
- hypertension
Additional factors include:
- high intake of refined vegetable oils,
- high intake of fats,
- high intake of mono- and polyunsaturated fatty acids,
- high intake of white flour based food products, and
- blue irises.
Clearly, some of these factors can be controlled, and others cannot. It still comes down to healthy diet, healthy body, better vision.
7. Get regular eye examinations.
Regular eye examination are a proactive approach to eye health.
Whether you have any of the risk factors listed above or not, what we all have in common is that we are getting older. Often patients don’t take action until they have noticed a change in vision.
Modern examination techniques have been developed to detect retinal and macular changes before patients are aware of a loss of visual acuity.
It is inevitable that as we reach the ages over 45, we will most likely need reading glasses. While this need for eyeglasses, called presbyopia, is not considered a disease, it does indicate that our visual system is aging. All adults should have a routine eye examinations every 18 months to 2 years. Those with special health concerns like diabetes, hypertension, and cardiovascular disease, should be examined every year. Once changes are identified, which indicate a disease process, examination will be more frequent.
Children should also receive eye examinations. There are those hereditary macular dystrophies, such as Stargardt’s Disease, Best’s disease, and juvenile retinoschisis, that affect children in the first and second decades of life.
Truth #7 Life does not end with the diagnosis of macular degeneration.
The concept of low vision often remains ambiguous to the general public, while the term ‘legally blind’ tends to be more widely recognized.
In reality, low vision encompasses a broad spectrum of sub-normal vision. It would be more accurate to define it based on an individual’s functional vision, which assesses the extent of disability by how effectively they utilize their remaining vision.
The objective of vision rehabilitation is to empower individuals with vision impairment to optimize their residual vision. This involves collaborating with eye care professionals and rehabilitation specialists to enhance independence and self-confidence. While rehabilitation therapy cannot restore lost vision, it aids individuals in utilizing their remaining vision more effectively. Ultimately, rehabilitation entails a process of acceptance, adjustment, and adaptation.
Acceptance
Life changes for sure. The changes are social, work related, financial, and psychological. The heaviest burden of vision loss is psychological. It affects your self-perception and social interactions. Acceptance is the psychological hurdle of understanding that things will never be the same. It is the attitude and understanding of how life will change that will determine success of rehabilitation
Adjustment
Things must be done differently. When you have a vision impairment, you start noticing how inconvenient life can be. Things seem to take longer, require more effort, your responses are slower, and actions need to be more deliberate.
Goals for schooling or employment will change. Activities you once enjoyed may change or be restricted. The independence you once commanded may now be curtailed. Adjustment is moving forward over all the hurdles of life. You may not be accepting of every change or challenge, but you just do the best you can do.
You might be interested in this other article ‘Adjusting to Vision Loss.’
Adaption
Adaption is developing skills and learning to use the tools and technology to get you to keep your life on track. These are skills, techniques, some optical and others non-optical that will be compensatory. It’s not easy. You must be willing to learn. This is by far the best time in history for those with low vision.
The rehabilitation process begins with identifying problems that you may be experiencing, then a program of problem solving is determined:
1. Management of the disease process
Optometrists, ophthalmologists, and primary care physicians have the job of educating you about the disease and its process. They help identify risk factors, associated health concerns, and implement treatments plans and monitor for progression. Get regular eye examinations and maintain a care regiment with your doctor.
The changes advised by the doctors may be related to lifestyle changes. Remember, diet and exercise; are the key to healthy body, healthy mind, and healthy vision.
2. Counseling
Therapists evaluate psychosocial issues of the persons psychological well-being and family related concerns. They are then able to provide counseling and referrals for guidance and education. They may also refer the individual to state and government resources and financial assistance.
3. Non-optical devices
Initially, those with vision loss find in the simplest things more difficult to do. These are the activities of daily living (often referred to as ADL.) Things like cooking, personal grooming, shopping, cleaning, and taking medications. These tasks can be made easier by implementing basic changes like lighting, increasing contrast and color, talking devices, and identifying by touch. These are non-optical aids. Occupational therapists help with setting up your home and work spaces for ease of use and training you in the use of both non-optical and optical aids.
4. Optical aids
First starts with an optimal pair of eye glasses as prescribed to you by your optometrist or low vision specialist. Those who work, go to school, or have specialized interests that require them to be able to see detail, will benefit from magnification devices. These are either standard magnifying lenses and telescopes or video magnifiers.
A low vision specialist will be able to help guide you through the many different types to help you select one most appropriate for the task. A rehabilitation therapist (occupational) will help train you to use these optical devices effectively.
4. Cutting edge technology.
Many with vision impairments have discovered that mainstream technology can be adapted to their needs. Smart phones, tablets, and virtual assistants like Alexa, Siri, Cortana,and Google Assistant are helpful.
Smartphone developers incorporated accessibility functions for large print, audio feedback, and lighting controls. Tablets have the same features and can be used for large print book reading. Software apps have been designed for navigating, reading aloud, magnification among other things.
Virtual assistants are voice controlled bypassing the need to see a screen or keypad. You can ask questions (time? date?), search the internet, and make phone calls. When connected to a smart home, functions of the home can be controlled with out seeing switches and dials. It can also provide security and notifications by audio alerts
Conclusion
Some aspects of the progression of macular degeneration can be controlled, others cannot. Arming yourself with the knowledge and a willingness to learn can determine your success to adjusting and adapting.
Learn about monitoring your macular degeneration in my other article: How to Monitor for the Progression of Macular Degeneration
The pessimist complains about the wind. The optimist expects it to change. The leader adjusts the sails. John Maxwell


