Studies have revealed a significant correlation between disabilities, such as vision loss, and the experience of depression and anxiety. Among the various disabilities, vision loss stands out as one of the most daunting, profoundly affecting daily life and playing a pivotal role in the onset of depression and anxiety. The fear accompanying the onset of vision loss often leads to negative attitudes and challenges in adjusting to a life with disability. Understanding this connection is crucial for developing effective coping strategies.
The Impact of Vision Loss on Mental Health: How vision loss can affect your life.
When considering the effects of vision loss, it’s necessary to look beyond the physical challenges and acknowledge the hidden burden it places on mental health. Depression and anxiety frequently accompany vision loss, yet these struggles often go unnoticed and untreated, affecting both adults and children alike.
Depression is a common experience, extending far beyond mere sadness. It can manifest as mild, intermittent episodes or as severe, daily occurrences. Recognizing and addressing persistent, functionally debilitating depression is important for improving overall well-being in those with vision loss.
The American Psychiatric Association in identifies major depression as having five of the following nine criteria:
identifies major depression as having five of the following nine criteria:
1. Depressed mood such as feeling sad, empty, tearful, or irritable most of the day, nearly every day;
2. Decreased interest or pleasure in most activities, most of each day;
3. Significant weight change (5%) or change in appetite;
4. Change in sleep: Insomnia or increased interest in sleep;
5. Change in activity: restless or lethargic;
6. Fatigue or loss of energy;
7. Feelings of worthlessness or excessive or inappropriate guilt;
8. Find it difficult to think or concentrate or an inability to make decisions; and
9. Thoughts of death or suicide, and
I would like to add:
10. Outbursts of anger, irritability, seemingly inappropriate for the situation.
While struggling with vision loss can be emotionally distressing, it’s the ensuing changes in daily functioning that often lead to frustration, depression, and anxiety.
The loss of vision significantly alters one’s quality of life, particularly among older adults. Depression can stem from feelings of diminished self-worth, a loss of independence, and an overall sense of losing control over one’s life.
This decline in quality of life creates a ripple effect on mental health, triggering a cascade of negative conditions. The mental well-being of an individual with vision loss can further diminish quality of life, potentially impacting their overall health and well-being significantly. Understanding these challenges is important for providing holistic care and support for those with visual disabilities.
Prevalence of Depression among the Visually Impaired
As the population of developed countries continues to age, there is a concurrent rise in vision impairments among older adults.
Numerous studies have highlighted a concerning trend: approximately one-third (1/3) of recently impaired adults experience clinical depression. This rate is twice as high as that observed in the same age group without vision impairments. The highest rates of depression are found among those who have recently lost their vision.
Understanding these statistics sheds light on the urgent need for targeted mental health support for individuals facing visual impairments.
Risk factors for depression:
Living alone. Feeling like a prisoner in your home due to insecurity about moving out of the familiar. Those with vision loss often suffer from social isolation.
Financial worries. Those that lose vision may have to stop working. There may be an increase in medical bills. Financial responsibilities may fall on another family member. These changes in the family dynamic can cause additional stress.
Vision loss at a relatively younger age (ages 40 -59)as opposed to older (>60). Most middle aged people are actively involved in work and activities. This vision loss is now an unanticipated obstacle and a hindrance to future plans and expectations.
Poor functional vision. How the individual feels about their vision and how they are able to function affects their mental status and level of depression. The increased level of frustration and depression results in lower visual functioning capability.
Unable to accept vision loss. Those that live with hope that somehow vision will return, that a treatment exists, or a miracle cure will arise. Those who do not accept and move on to adjusting and adapting are susceptible to depression.
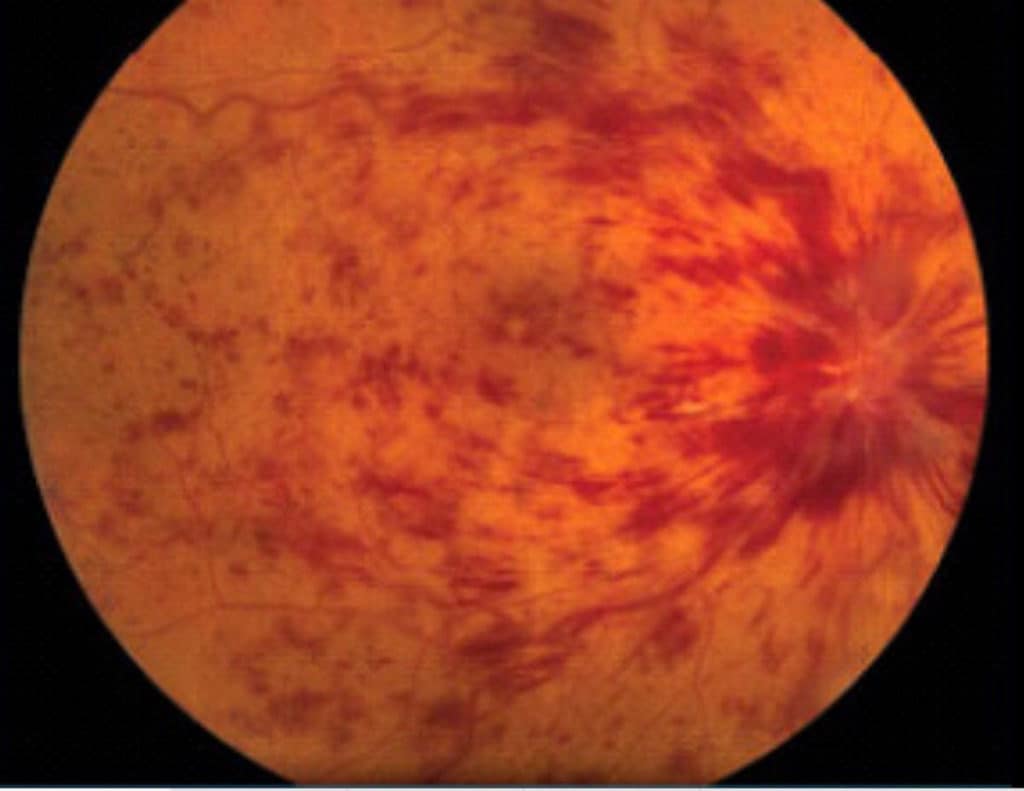
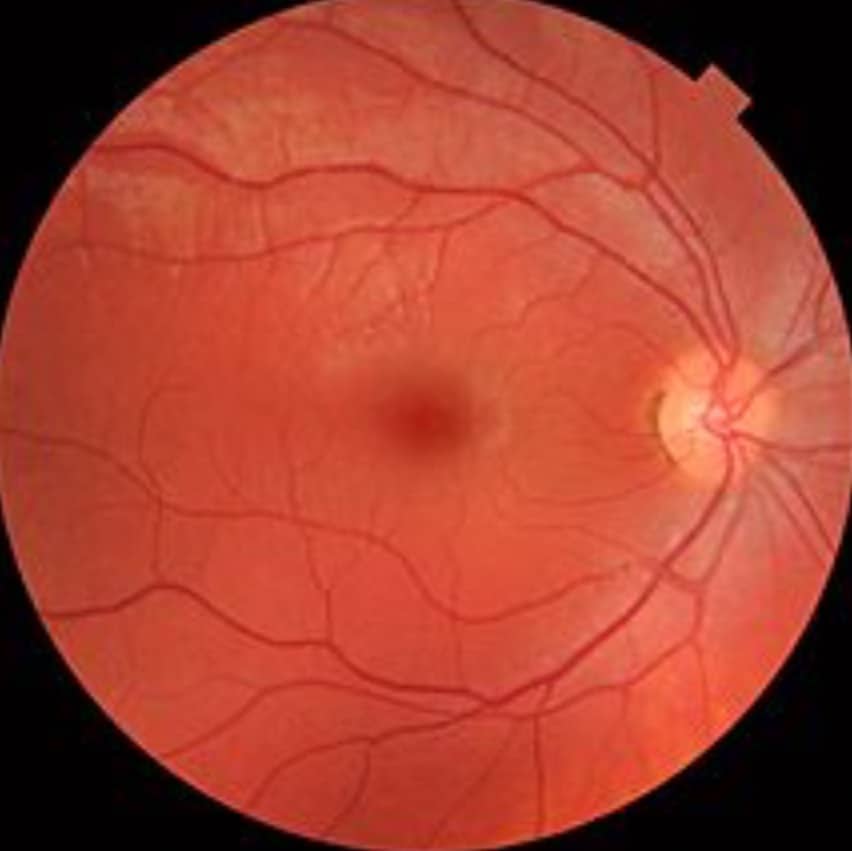
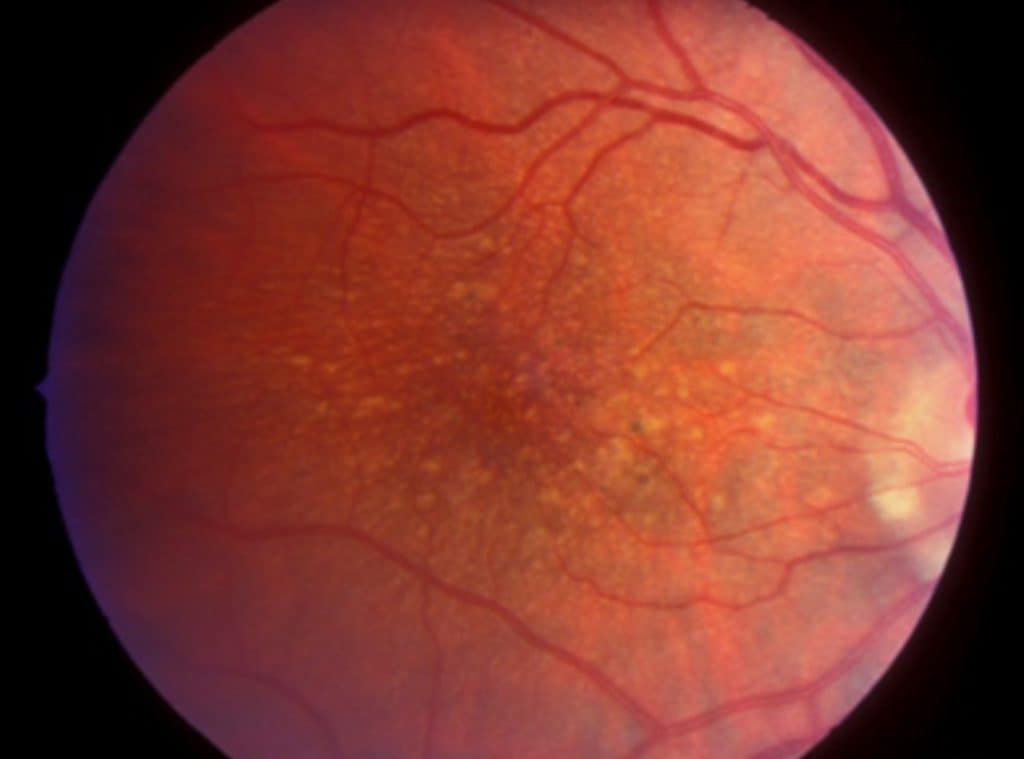
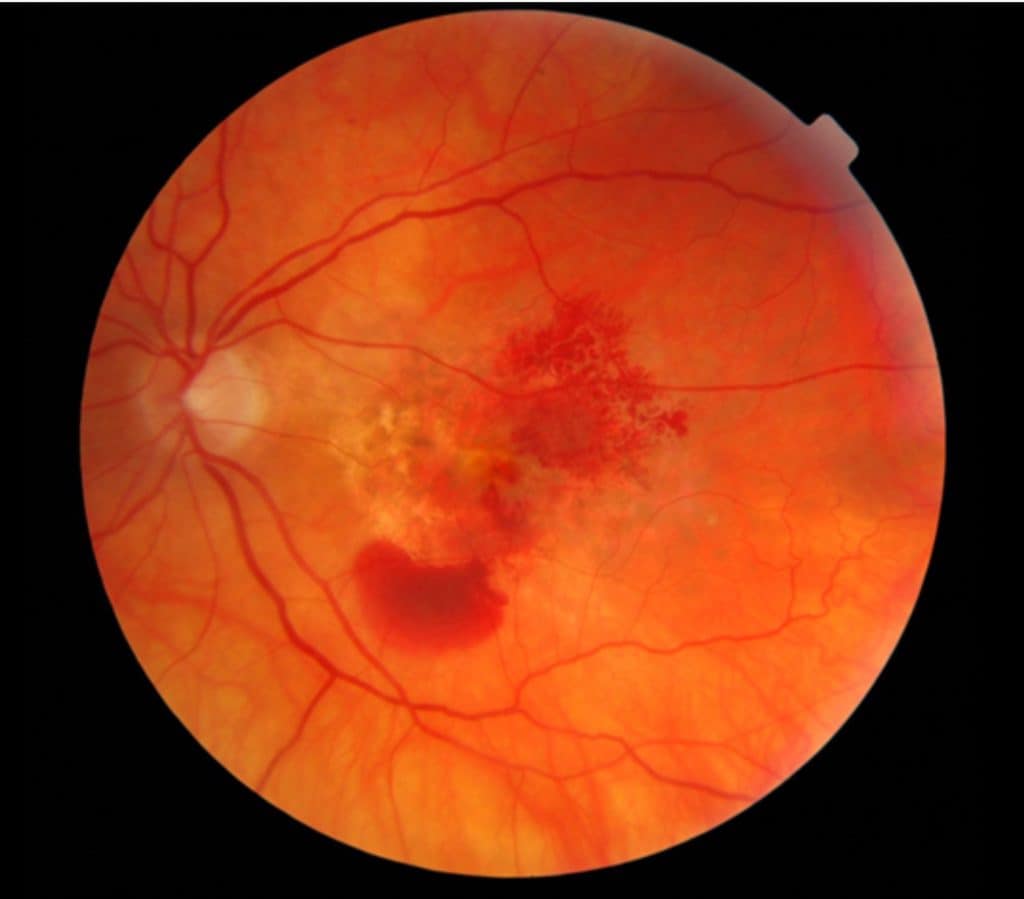
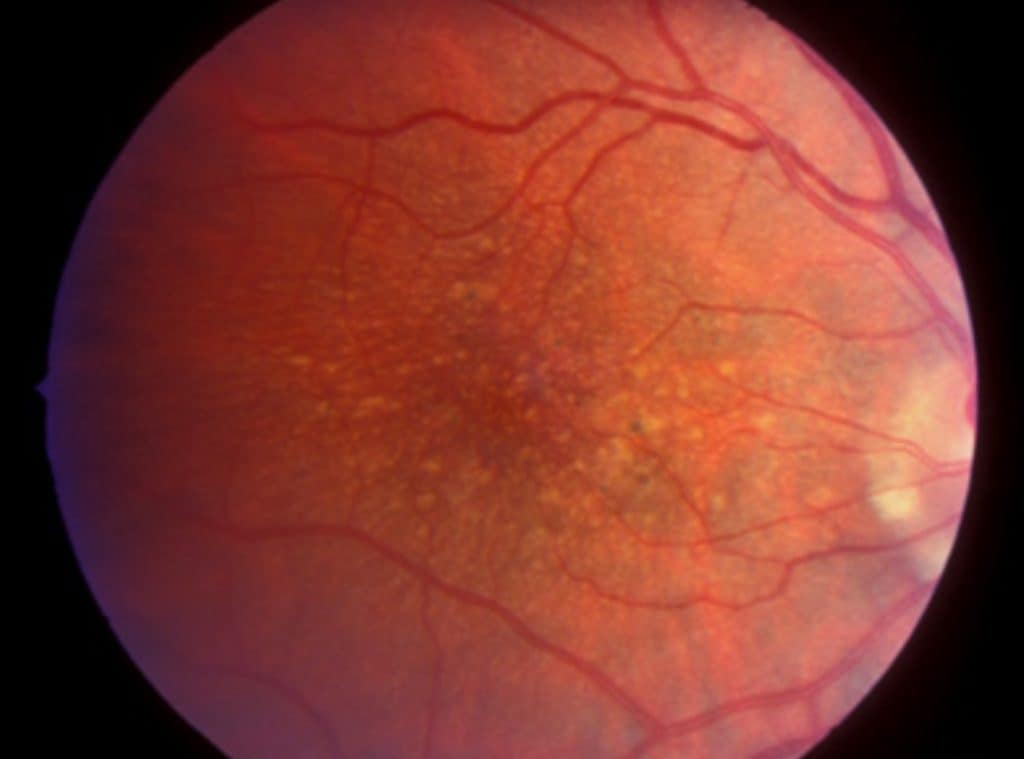
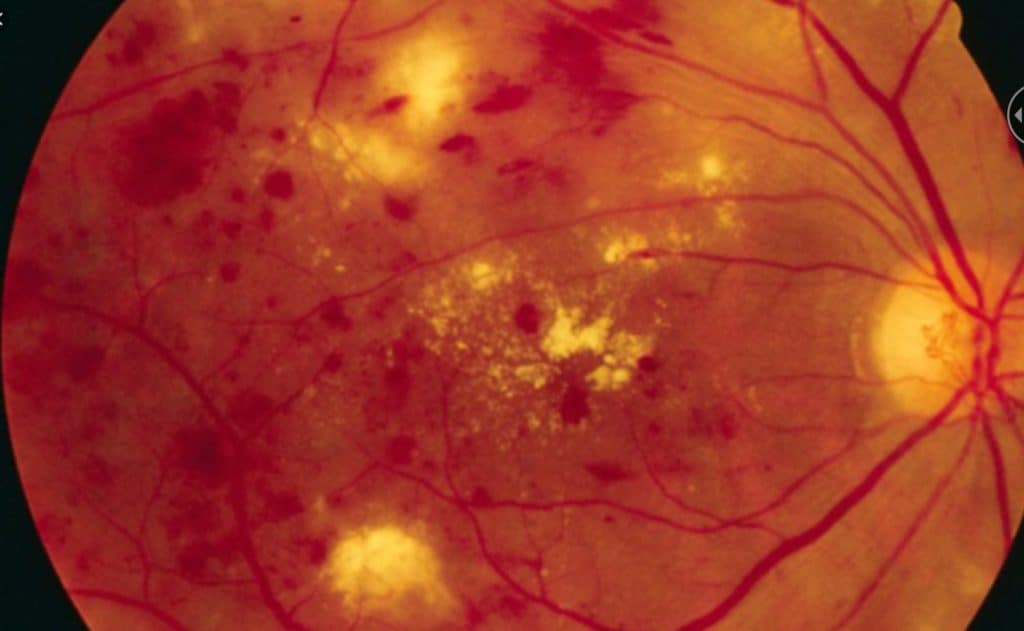
Macular degeneration. AMD is the most common cause of low vision in adults over the age of 60 in the developed countries.
Other health problems. Poor physical health in and of itself is a risk factor for depression. Sight loss can be a compounding factor placing additional restrictions on activates and work.
Ref: Depressive symptoms in people with vision impairment: …BMJ open
Anxiety
Anxiety often walks hand in hand with depression, presenting its own set of challenges. Much like depression, anxiety can persist and manifest in various forms. It encompasses worries, both big and small, affecting behaviors and the willingness to adapt.
Minor fears might deter you from exploring new opportunities. Loss of confidence and frustration over small mishaps, such as pressing the wrong button on a stove or avoiding using a TV remote out of fear of making an irreversible mistake, are common experiences.
On a larger scale, anxiety can lead to isolation and avoidance of social interactions. Fear of social judgment or pity, apprehension about traveling alone, and the dread of social embarrassment due to misunderstood actions can become overwhelming.
The inability to read non-verbal cues, such as body language or facial expressions, adds to this anxiety. Feeling adrift, unaware of subtle details or visual jokes, can create a sense of being “alone in a crowd.” Small embarrassments may amplify the anticipation of others’ judgments regarding one’s capabilities and limitations, leading to avoidance of social situations— a form of self-isolation.
Learn more about low vision and problems with facial recognition in my other article: Why Those with Low Vision have a Problem with Facial Recognition
The greatest fear looms: blindness. Often, others fail to grasp the complexities of this disability, especially when individuals with visual impairments can function normally in most situations (a concept known as ‘passing,’ which I discuss in another article). Falling short of these perceived expectations, even if only apparent to oneself, can significantly impact self-esteem and heighten anxiety levels. Understanding and addressing these anxieties are steps towards holistic well-being for the visually impaired.
In her classic book, Clinical Low Vision, Dr. Eleanor Faye was able to best describe the dilemma of the visually impaired:
“The terms “sighted” and “blind” represent groups possessing well established stereotypes and culturally expected rules of behavior. The position and role of the partially sighted person is much less clear owing to the tremendous range of variability in partially sighted types. Generally society views them as sighted and expects them to function as such.”
Want to learn more about ‘passing,’ see my other article: Pretending not to be Visually Impaired: Passing with a Disability
Depression and Anxiety in Visually Impaired Children
Children who acquire low vision may struggle to articulate their concerns or the challenges of their disability to others. Their understanding of their differences may not be clear, adding complexity to their emotional development.
These early years are crucial for self-perception and identity formation. How others treat them plays a pivotal role. The visually impaired child might perceive themselves as ‘slow’ or ‘dim’ due to the way adults, especially those unfamiliar with the disability, may overly assist them. This can lead to a lack of confidence and insecurity about their capabilities.
Sighted children, observing the low vision child’s behaviors such as holding objects close, using magnifiers, or thick glasses, may engage in teasing or ridicule, as children often do. The limitations in participating in activities that sighted children take for granted can further contribute to low self-esteem and self-worth in these young individuals.
Additionally, children are perceptive to their parents’ anxieties. Parents, understandably concerned and seeking assistance, can inadvertently transfer their fear and worry to their child, amplifying the child’s own sense of anxiety and insecurity. Understanding these dynamics is important for providing effective support and fostering positive self-image and emotional well-being in visually impaired children.
Like adults, persistent sadness or persistent fears can be signs of depression and anxiety. The child may not be able to express their feelings. Watch for signs of anxiety.
- Irritability,
- fear of school and social situations.,
- fatigue, or
- trouble sleeping,
- stomachaches, and
- nausea.
Signs of depression are similar to adults:
- Persistent sadness,
- reluctance to participate in activities,
- changes in eating patterns – eating a lot more or a lot less than usual,
- changes in sleep patterns – sleeping a lot more or a lot less than normal,
- low or overly agitated energy level– being tired and sluggish or tense and restless a lot of the time,
- having a hard time paying attention,
- low self-esteem, low self-confidence.
Ref: Centers for Disease Control and Prevention
Supporting Your Visually Impaired Child Through Depression and Anxiety
Life with a vision impairment is far from the end of the road. Countless stories exist of blind and visually impaired individuals excelling in college, pursuing fulfilling careers, and even competing in the Olympics.
Empower your child to find their own solutions to challenges. Encourage them not to let their disability become an excuse that holds them back. While it’s essential to provide love, affection, and moral support, avoid dominating their life with excessive assistance. Encourage them to connect with groups of friends or support groups to develop social skills and coping mechanisms. With your guidance, they can learn to navigate the challenges they face.
Consider seeking the assistance of qualified therapists who specialize in supporting children with visual impairments. These professionals can help both you and your child gain a deeper understanding of their emotions and provide valuable strategies for managing depression and anxiety. By working together and fostering independence, you can empower your visually impaired child to thrive and embrace a fulfilling life.
A reader made a recommendation for an article that takes a deeper dive into Teenage Depression
Addressing Depression in the Visually Disabled: The Treatment Pathway
Treating depression in the visually disabled community can be challenging as it often goes undetected and untreated. There is a reluctance to acknowledge depression, perhaps due to the stigma surrounding mental health issues, or the misconception that it’s an inevitable part of aging with no definitive cure. Some individuals may find it difficult to seek help if they deny their feelings, dismissing them as just temporary sadness.
It takes a village
Successful treatment typically involves a comprehensive approach, starting with a low vision evaluation conducted by a specialized professional such as a low vision specialist, often an optometrist. Additionally, a rehabilitation therapist—usually an occupational therapist trained in low vision rehabilitation—can provide valuable assistance. In some cases, a psychiatrist trained in counseling individuals with disabilities may also play a important role in developing a holistic treatment plan. This multidisciplinary approach ensures that the individual receives the tailored support needed to address their depression effectively.
Tips on coping with vision loss, read my articles: How to Adjust to Vision Loss, 7 Keys to Coping
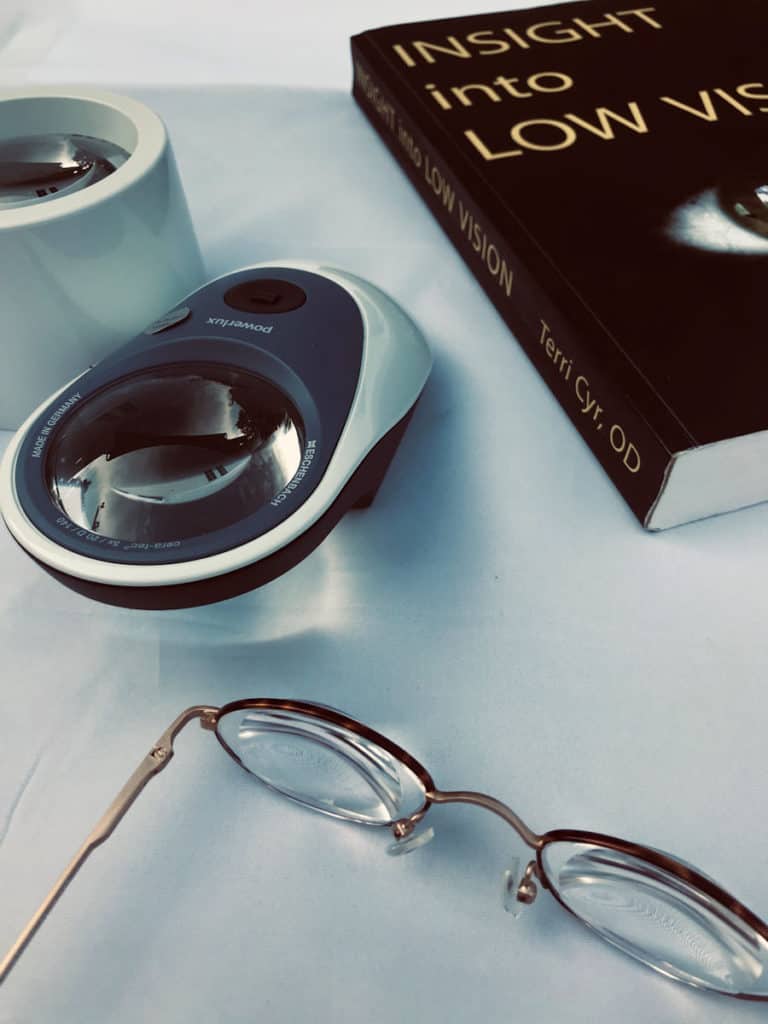
Low Vision Evaluation
A low vision evaluation serves as a pivotal tool for problem-solving in the journey of those experiencing depression or anxiety due to vision loss. It offers individuals the opportunity to explore and regain functional capabilities, focusing not on treating the disease itself with medications or surgery, but on developing new strategies to adapt to vision loss and enhance the functionality of their remaining vision.
Here are the reasons to get a low vision evaluation;
1. To Advocate for Yourself;
2. Introduction to Visual Aids and Techniques;
3. Education and Counseling, and
4. Appropriate Referrals.
The primary aim of a low vision evaluation is to improve the individual’s quality of life. By increasing functional residual vision, the evaluation helps rebuild self-confidence and motivation for adjustment. This process involves exploring a range of new technologies and both optical and non-optical aids that can empower the visually impaired to regain independence and take more control over their life. Through this evaluation, individuals can discover tools and techniques tailored to their specific needs, facilitating a more fulfilling and independent lifestyle despite their visual challenges.
I like to think that technology makes things easier and makes things possible.
See my other article:
6 Reasons Why the Visually Impaired Refuse Low Vision Aids
As wonderful as all this new assistive technology is, it may not solve all the issues associated with depression and anxiety.
Rehabilitation: A Path to Renewed Independence
Rehabilitation for individuals with vision loss is a transformative journey aimed at empowering them to navigate life in new ways. This process involves learning innovative skills to promote independence and bolster feelings of self-worth. The goals of rehabilitation must align with the individual’s aspirations, going beyond merely teaching skills to someone who may be struggling with motivation due to depression and anxiety.
The essence of rehabilitation is about more than acquiring techniques; it’s about resetting one’s approach to life. Through this process, individuals discover new ways to accomplish tasks and pursue activities they once enjoyed. By focusing on personalized goals, rehabilitation becomes a catalyst for building confidence and embracing independence.
This holistic approach not only equips individuals with practical skills but also helps them rediscover a sense of purpose and fulfillment in their daily lives.
See my other article : Why the visually impaired resist therapy
Psychotherapy for Emotional Support
Psychotherapy, guided by a qualified therapist, offers valuable support for managing interpersonal challenges and family dynamics. A therapist can assist in identifying and addressing social interactions, helping individuals cope with others’ perceptions of their disability, and navigating feelings of grief and sadness associated with their situation. Therapy serves as an important tool for facilitating the transition to a new life as a person with a disability.
Equally significant is the benefit of family counseling, as the dynamics within a family unit often undergo changes with the introduction of a disability. Living with a disabled family member can place strain on relationships, leading to stress, resentment, anger, or anxiety.
Joint counseling sessions provide a space for both family members and the disabled individual to navigate these changes together. By addressing these emotional challenges collaboratively, families can work towards understanding, acceptance, and improved communication, fostering a healthier and more supportive environment for all involved.
Additional article on fear, depression, anxiety, and secondary gain: Why the Visually Impaired Resist Therapy
In the End;
Depression and anxiety are all too common among individuals with visual impairments, yet they often remain undetected or untreated. Rehabilitation and treatment for vision loss, mental health concerns can easily take a backseat, with the assumption that addressing physical impairments will solve everything. This oversight can leave those struggling with depression and anxiety feeling unheard and isolated.
Advocate for yourself when it comes to mental health services. If these services are not offered to you, seek them out. There is no shame in asking for help. Depression is a recognized aspect of acquired disability, as well as aging, and treatment can be an important step towards regaining a sense of well-being and a fulfilling quality of life.
Remember, your mental health matters just as much as your physical health, and seeking support is a courageous step towards a brighter tomorrow.

He is a wise man who does not grieve for the things which he has not, but rejoices for those which he has. Epictetus (Greek Stoic philosopher)