Researchers have studied Mirtogenol®, Ginkgo biloba, marijuana, baicalein, and forskolin for their anti-oxidant, anti-inflammatory, neuroprotective, or eye pressure lowering effects, as natural glaucoma treatment alternatives to pharmaceutical drugs.
Glaucoma is a general term, used to describe numerous subgroups of the eye disease that result in optic nerve damage. The simple definition is that it is a disease of high eye pressure, but it is actually more complicated than that.
The eye is constantly manufacturing fluid in the anterior chamber of the eye. This fluid continually flows out of the eye by way of the blood stream. Glaucoma is a problem of reduced blood flow to the tissues of the eye. The decreased blood flow causes a disruption in the flow of the fluid out of the eye. Fluid not filtered out of the eye causes an increase in intraocular pressure (IOP.) Increased intraocular pressure (IOP) is a major risk factor for the damage to the nerves of the eye. This high eye pressure form of glaucoma is commonly called Primary Open Angle Glaucoma (POAG.)
But it is not the only risk factor. Poor small blood vessel circulation, especially at the level of the optic nerve and oxidative stres, are also risk factors. The type of glaucoma which is not characterized by high eye pressure is called Normal Tension Glaucoma (NTG.)
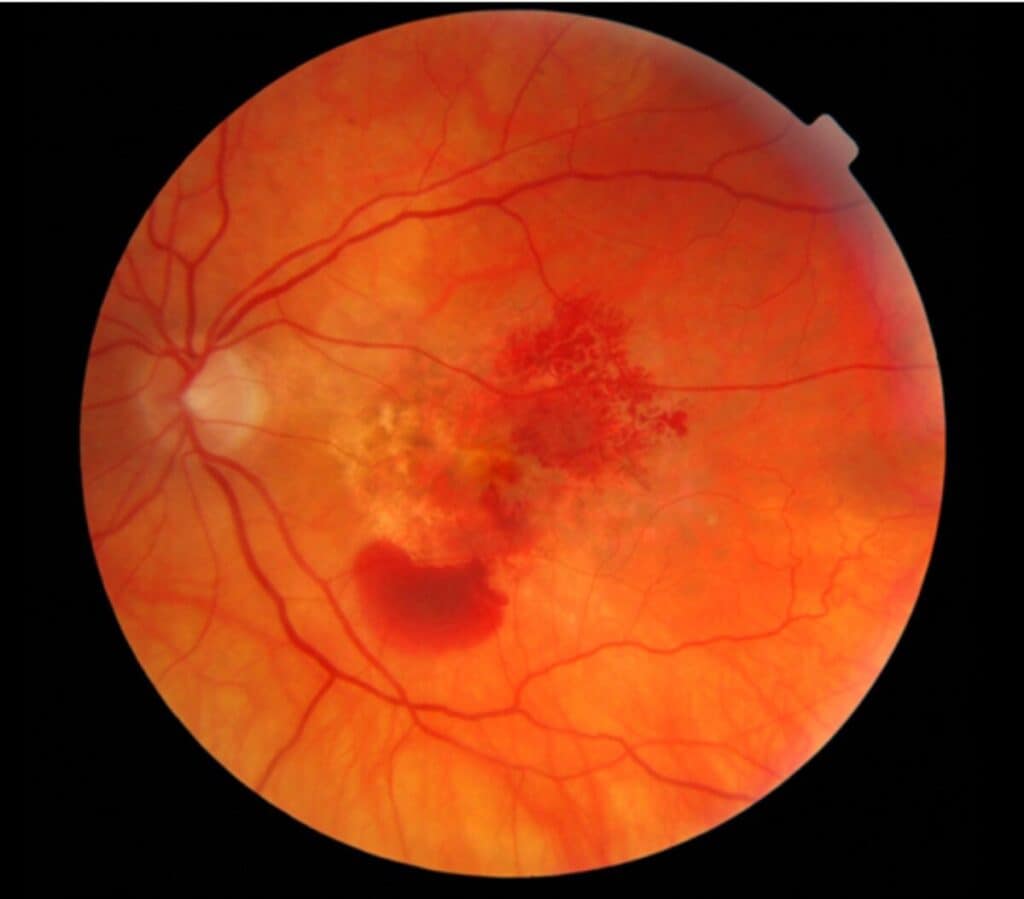
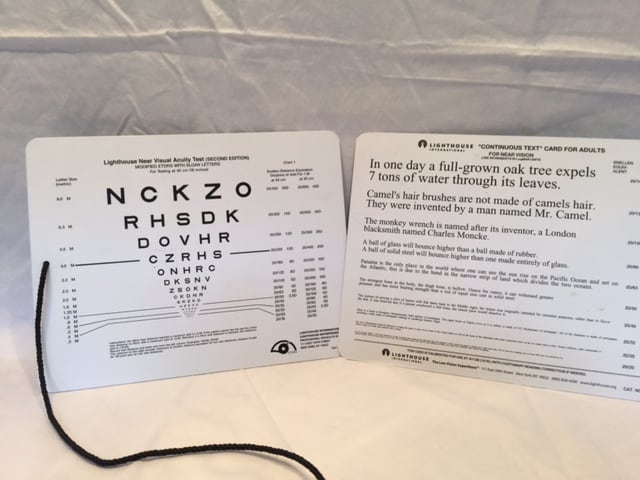
The damage of glaucoma is evident at the optic nerve, which is where the light-sensing retinal ganglion cell axons come together to form the optic nerve and exit the orbit of the eye on their way to the brain. Death of these cells initially results in visual field loss, followed by loss of visual acuity.
Glaucoma is chronic, progressive, lifelong, and potentially blinding if not treated.
The management and treatment goals of treating glaucoma are to slow the progression and stabilize the visual field loss.
In the early stages of glaucoma, the treatment of choice is eye drops. While there are several different categories of medications, eye drops function in one of two ways:
* Decrease the production of aqueous fluid, (ex: beta-blockers); or
* Increase outflow of fluid, (ex: prostaglandins).
The taking of eye drops is lifelong and can be expensive. Patients, very often, dislike taking eye drops. It does not cure glaucoma. These treatments manage glaucoma.
Patients often ask if there is natural dietary supplements for glaucoma as an alternative to eye drops, lasers, and surgery. Searching through the literature, I found 5 natural dietary supplements that claim to control glaucoma. They are:
1. Mirtogenol®: which is Bilberry and French Maritime Pine Bark extract
2.Ginkgo biloba
3. Marijuana
4. Baicalein
5. Forskolin
1. Eye Pressure Control: European bilberry + French Maritime Pine= Mitrogenol®
Mirtogenol is named for the combination of Mirtoselect® and Pyrogenol®. Mirtoselect® is bilberry extract and Pyrogenol® is French maritime pine bark extract.
Bilberry is a darkly pigmented berry found in northern Europe, which is high in anthocyanins. Anthocyanins are flavonoids, which are the blue-black pigments of bilberry. These flavonoids have anti-oxidant and anti-inflammatory bioactivity. Bilberry extract is also thought to have a neuroprotective (protects nerves from damage, degeneration, and impairment) function to enhance the stability of retinal ganglion cells and the optic nerve. While it has many potential benefits, anti-oxidant, anti-inflammatory, and is neuroprotective, it does not decrease eye pressure.
Researchers are also evaluating anthocyanins for their blood pressure lowering, blood lipid (LDL) lowering, and blood sugar lowering effects. Bilberry has long been associated with vision benefits. Studies have shown that bilberry and vitamin E together have been successful in decreasing the progression of cataracts. It has not been proven, by clinical studies, to increase night vision.
The extract called Mirtoselect® is a highly purified anthocyanin-rich extract, devoid of the non- anthocyanin components.
Pycnogenol® is a standardized plant-based extract obtained from the bark of the French maritime pine. This is a brand used by research studies because of its known purity. It has strong anti-oxidant, anti-inflammatory, and capillary protective activity (this could be significant for those with diabetic retinopathy.) Interestingly, the use of pine bark as an anti-inflammatory goes back to the time of Hippocrates.
Mirtogenol® is a combination supplement trademarked by Indena, Milan, Italy and Horphag Research, London, UK.
In a study , Mirtogenol® lowered IOP in those at risk for developing primary open angle glaucoma (POAG.) The mechanism is the combined activity of the two extracts to increase blood flow through the tiny blood vessels of the eye. By increasing blood flow the inflow and outflow of fluid stabilizes eye pressure.
Who should take Mirtogenol®?
Supplements with Mirtogenol® are indicated for those with elevated eye pressure and are at risk for developing glaucoma.
Dosage of Mirtogenol®
The dosage given in the study (referenced below) was Pycnogenol® 40 mg and Mirtoselect® 80 mg, twice a day. The full eye pressure control effect was reached at 3 months. Reviewing commercially available ‘Eye Pressure Control’ supplements with Mirtogenol® lists the dosage at 120 mg (40mg + 80mg.) The indication is to take with food to prevent gastric upset.
Safety
Both of these extracts, Mirtoselect® and Pycnogenol® have been used for decades as a dietary supplement without reported side effects.
Precaution recommends that Pycnogenol® is not for children under 6 years of age and should not be taken during the first 3 months of pregnancy.
(Ref: Effects of Mirtogenol® on ocular blood flow and intraocular hypertension in asymptomatic subjects
2. Ginkgo biloba as a Natural Treatment for Glaucoma
Ginkgo bil0ba are extracts from ginkgo biloba leaves that have been used for centuries in Asian medicine. The extracts are comprised of flavonoids and terpenoids. It is credited to be an anti-oxidant, anti-inflammatory, and neuroprotective (protects nerves from damage, degeneration, and impairment.) Neuroprotection is essential for those with glaucoma, because it is the loss of retinal ganglion cells that results in vision loss.
Ginkgo biloba is also effective in promoting small blood vessel circulation. Gingko biloba does not have an effect on eye pressure. It is thought that it is this capability to increase ocular blood circulation and its neuroprotective effect that slows the progression of glaucoma.
Because of these bio-active effects, ginkgo biloba can be beneficial for prevention and treatment of other eye diseases such as diabetic retinopathy, macular degeneration, and cataracts.
Who should be taking Ginkgo biloba?
Researchers have found that Ginkgo biloba has potential to treat those with glaucoma caused by other risk factors besides high eye pressure. (Remember, Ginkgo does not affect eye pressure.) This is significant for those with eye pressure in the normal range, but are still experiencing retinal ganglion cell damage (also known as Normal Tension Glaucoma.) In these cases of progressive normal tension glaucoma, it may be taken as a adjutant to medical therapy.
Recommended Dosage of Ginkgo biloba
Research studies most commonly used 40 mg extract, three times a day, for a total of 120 mg per day. Reviewing commercially available supplements, the dosage given is 40 mg, 60 mg, or 120 mg. Extrapolating from research dosages, it would be 40 mg/3 times per day, or 60 mg/twice a day, or 120 mg/ once a day.
Safety of Ginkgo biloba
There have been reported incidents of spontaneous bleeding for those at risk (risk factors like; other medications, old age, liver cirrhosis), who are simultaneously taking non-steroidal anti-inflammatory drugs (NSAIDs. ex; hi-dose aspirin, ibuprofen, naproxen) and anticoagulants such as Plavix, heparin, or warfarin. However, several studies could not implicate the combination treatment as the cause of bleeding. Overall, Ginkgo biloba has a good safety profile. It is always a good idea to discuss supplementation with your physician before launching into a new supplement regiment.
(Ref: Ginkgo biloba: An adjuvant therapy for progressive normal and high tension glaucoma )
)
3. Marijuana as a Natural Treatment for Glaucoma
Marijuana is the dried leaves and stems of the Cannabis sativa plant. Historically, it has been used as a recreational substance for its psychotropic effects. It can be smoked or eaten (usually in baked goods), or drank as a tea.
It’s significant extracts are ∆-9-tetrahydrocannabinol (THC) and cannabidiol (CBD). It is the THC which is smoked, vaporized or taken orally for recreational use. This active ingredient, over stimulates brain cell receptors. This is how the desired ‘high’ occurs for recreational users.
The mechanism by which marijuana lowers eye pressure is not fully understood. Clinical data suggests that it may suppress aqueous fluid production and increase fluid outflow from the eye. It is also thought to have a neuroprotective effect.
THC based medications ( Marinol) have been approved by the FDA as a treatment for nausea and appetite enhancement for cancer patients undergoing chemo-therapy and those with wasting diseases like AIDS. Another extract, CBD (there is an estimated 80 cannabinoids in marijuana) has been approved for a form of childhood epilepsy. THC and CBD (2 of the many cannabinoids ) combined with other medications are formulated to treat spasticity and neuropathic pain.
Safety and Side Effects of Treating Glaucoma with Marijuana
The marijuana plant has many other botanical compounds as a part of its structure. It is these other compounds that can cause problems and adverse side effects when smoked or eaten.
Short-term effects, besides the ‘high’ are; reduced blood pressure, increased heart rate, anxiety, and paranoia. Eyes become red and dry. The pupils of the eyes become small and light sensitive.
Consider, if the problem of blood flow to the eye is a risk factor for glaucoma, the reduction in blood pressure is counter to the benefit of lowering the eye pressure.
Long term use (years) can affect thinking, memory, and learning capability. Physically, frequent smoking of marijuana can irritate the lungs and increases the risk for substance abuse disorder. It should not be used during pregnancy. It has been credited for creating behavioral problems in these children. (Ref: Marijuana Drug Facts )
)
Who Should Be Taking Marijuana to Treat Glaucoma?
Several studies have shown that the THC and other cannabinoids ‘significantly’ reduce eye pressure in both glaucoma patients and normal healthy individuals.
It was discovered 40 years ago that smoking marijuana decreased eye pressure (chief risk factor of glaucoma.) However, since that time, better therapies for treatment have been developed, which do not have the side effects of either smoking or ingesting marijuana.
At this time, there are no cannabinoid medications approved for treatment of glaucoma. The American Academy of Ophthalmology and the American Glaucoma Society do not recommend the use of marijuana to treat glaucoma.
Dosages of the Cannabinoids
The effectiveness of the cannabinoids is dependent on the dose, but is generally short-lived, 3 – 4 hours. Because it has a short-life of effectiveness, it must be taken frequently.
This need to keep smoking or ingesting marijuana is not conducive to good ocular eye pressure control. Contemporary pharmaceutical treatments, which are effective without the side effects, need to only be taken once or twice a day.
The future of treating glaucoma with marijuana requires more clinical research to isolate the eye pressure lowering component (cannabinoids), which can be used as a glaucoma treatment without the adverse side effects. (Ref: Herbal Medicines in Glaucoma Treatment )
)
The next two herbal supplements are less well known as natural treatments for glaucoma:
4. Baicalein
Baicalein isolated from the Chinese medicinal herb, Scutellariae radix (Blue baikal Skullcap a.k.a. Chinese skullcap). This active compound has been widely used in Asian countries for the treatment of many diseases. It is a flavonoid compound and like most flavonoids, it has powerful anti-oxidant, anti-inflammatory, and neuroprotective activity. (Flavonoids have also been proven to decrease cataracts and AMD.)
Pharmaceutical eye drop treatment for glaucoma focuses on reducing eye pressure. The studies on baicalein, thus far, have been animal studies (gerbils) and have shown that when introduced systemically, it reduced eye pressure. Although research is ongoing, it is thought that baicalein reduces eye pressure in two ways:
1. decreasing aqueous humor production at the ciliary body, and
2. it has been shown to facilitate the mechanism of outflow, leading to IOP reduction.
It is anticipated that this supplement will be used as an adjuvant treatment for glaucoma in combination with standard glaucoma medications.
Safety of Baicalein
Baicalein has been used in traditional Chinese medicine with no recorded side effects. Still little has been done with safety and effectiveness in human clinical studies. (Ref: ARVO )
)
5. Forskolin
Forskolin is extracted from the root of the Indian Coleus, which is a plant from the mint family found all over India. Recently, it has gained fame as a dietary substance for weight loss.
The mechanism of action favorable for eye pressure control is thought to be it’s ability to suppress the formation of aqueous fluid.
There are very few studies of forskolin as a treatment for glaucoma. It was first studied in the 1980’s when it was revealed to lower eye pressure in a small group of healthy patients. The most significant and hopeful study was one done in India. Subjects used a 1% eye drop solution of forskolin three times a day. The study indicated a 4 to 5 mm Hg average reduction in eye pressure.
Other studies administered forskolin as an oral supplement combined with flavonoids. This was less conclusive than the eye drop study because of the inclusion of flavonoids, which we know have anti-oxidant and anti-inflammatory, and are neuroprotective favorable for controlling glaucoma. So the role of forskolin is less clear.
Safety of Forskolin
There is only limited information about any long term side effects. Those who took the eye drops experienced some transient redness and/or irritation.
Forskolin oral supplements have been shown to decrease heart rate and lower blood pressure. So those taking blood pressure medications should not take forskolin. It is also recommended that those on anticoagulants and anti-platelet therapy should also avoid forskolin. There is evidence that it has androgenic activity on cells of the prostate and should be avoided by those with prostate cancer.
Dosage of Forskolin
Those in the Indian study administered 2 drops of 1% forskolin 3 times a day. (This formulation is not available for purchase at the time of this writing.) The multiple of times (3 x per day) that the drops must be instilled detracts from its desirability as an alternative treatment.
Who Should Take Forskolin?
Forskolin has the potential to be a new class of glaucoma treatment. The study out of India suggested that it may be a good alternative medication for those with asthma who cannot take beta-blockers (timolol.) ( Ref: Efficacy and safety of 1% forskolin eye drops …)
…)
Right now, I would say to wait until more studies are done to prove its safety and effectiveness.
In the End…
Keep in mind that the FDA evaluates and regulates prescription drugs and those drug treatments sold over-the-counter, but they do not regulate herbal medications and nutritional supplements. For that reason, safety and efficacy studies are not required. Therefore, herbal and nutritional supplements may vary in purity and potency.
None of the mentioned herbal supplements have the potential, at this time, to have the same efficacy as current glaucoma eye drop medications for lowering eye pressure. There is some potential for their neuroprotective effect which reduces the loss of the retinal ganglion cells critical for maintaining vision. Most studies suggest that these supplements (predominantly Ginkgo biloba, bilberry, and Mirtognenol®) should be considered as adjuvant to standard prescribed glaucoma medications.
The effectivity of these natural dietary supplements to control and treat glaucoma need larger and more in-depth studies to better gauge their potential.
Can a Cup of Hot Tea a Day, Reduce the Risk for Developing Glaucoma

The on-line British Journal of Ophthalmology published a report indicating that “Drinking a cup of hot tea at least once a day may be linked to a significantly lower risk of developing the serious eye condition, glaucoma.”
The investigators looked at an American study which yearly, surveys the lifestyle and health status of 10,000 Americans, by means of both physical exams and interviews.
The researchers looked at the subjects consumption of coffee, tea, and soft drinks, both with caffeine and without caffeine. After sorting through and teasing out the data (I won’t bore you with the numbers here), the investigators determined that the drinking of a cup of hot tea with caffeine daily reduced the risk of developing glaucoma by 74%. In health research 74% is a BIG number. An almost Too-Good-to-be-True number.
So what is it? Why would the caffeinated tea reduce the risk, but not the caffeine in coffee or soda? For that matter, de-caffeinated tea was not a factor in reducing the risk, at least not in this study. The American survey did not delve into types of tea (green tea, black tea,, Oolong tea, Lipton tea), brewing times, size of the cup, etc. The information was general: one cup (or more) daily.
Glaucoma is a progressive, sight threatening eye disease. The common understanding is that it is a disease of high eye pressure, that damages the light sensing neurons of the retina of the eye. The progressive damage to these nerves results in nerve cell death, and subsequent loss in vision. Most therapies are centered on controlling the pressure inside of the eye. But doctors are finding that these therapies are sometimes not enough. Medical research is focusing on other factors that contribute to the progression of glaucoma.
So that brings us back to the role that hot tea may play in reducing the risk of glaucoma. The questionable aspect is the caffeine. Other research has shown that the eye pressure can go up, which is undesirable, when caffeine, in the form of coffee, is ingested. (Ref: JGlaucoma )
)
Tea has other beneficial factors, such as antioxidants, anti-inflammatory, and neuro-protective substances. These factors are also essential for good general health. They have been studied as an important nutritional component for heart and vascular health, diabetic control, and cancer prevention. That which is good for the body is good for the eyes.
The researchers conclude that more research needs to be done to sort out the effects of tea on the risk for the development of glaucoma.
You may also be interested in…How Caffeine Affects Eye Disease and Causes Visual Disturbances