Individuals with vision impairment often adopt behaviors and tactics to hide their disability, striving to blend in and appear “normal.” This is facilitated by the fact that vision impairment is often categorized as an “invisible” condition.
What is Passing?
“Passing” in the context of disability refers to the intentional act of concealing one’s disability. It involves individuals with disabilities attempting to appear as if they do not have a disability, especially in social situations. This can involve hiding behaviors or characteristics associated with their disability to blend in with able-bodied individuals.
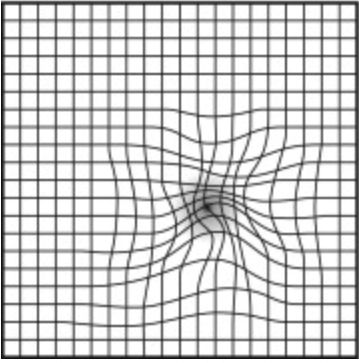
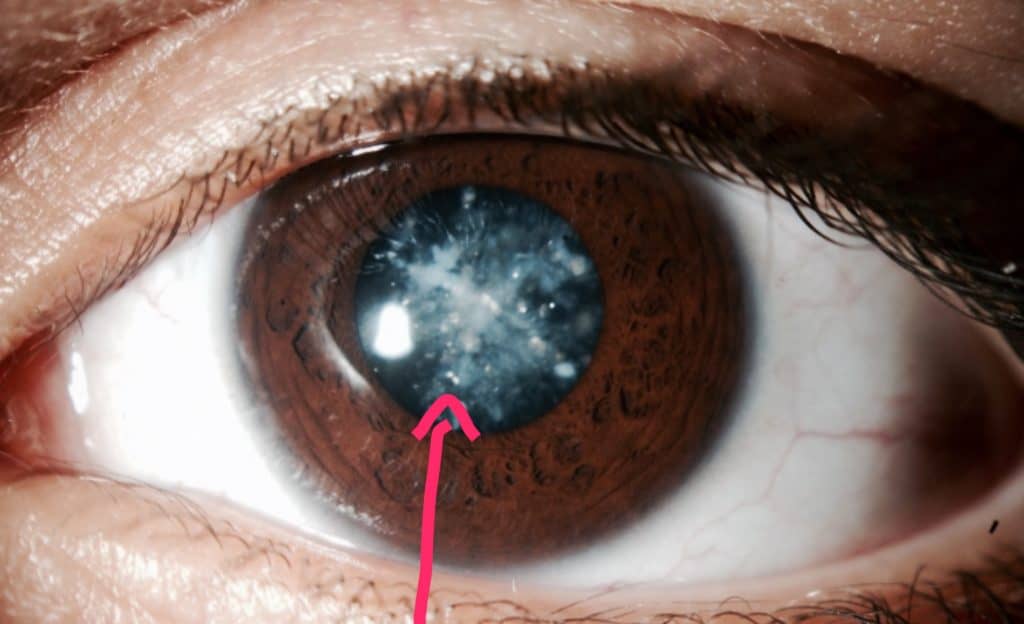
Vision impairment is often considered “invisible” because it may not be immediately apparent to others when interacting with someone with this disability. There are typically no outward signs of vision loss unless a person exhibits specific low vision behaviors, such as holding objects very close, tilting their head, excessive blinking, or eye movements that appear unfocused or exaggerated.
Passing may seem deceptive or dishonest to some, as individuals are essentially pretending to be able-bodied when they are not. However, for many with vision impairment, the decision to pass as fully sighted is deeply personal and often driven by emotional reasons.
Living in a world between the blind and the sighted, those with visual impairment often use passing as a form of self-defense. It allows them to create a façade of normalcy, helping to protect their social acceptance and preserve their psychological well-being.
Why the visually impaired conceal their disability.
Social Pressure: The social stigma attached to the term “disability” can subconsciously compel those with invisible disabilities to conceal their condition, aiming to sidestep the negative social implications of deviating from what is considered “normal.”
Lack of Understanding: Many individuals without visual impairments may not fully comprehend what “low vision” entails. Social norms often equate disability with a perceived lack of capability, extending beyond just the ability to see. Vision impairment is sometimes mistakenly equated with blindness or even intellectual disability.
They may find it is just easier to pretend. Openly identifying themselves as disabled, means opening up the “I can’t see, but I’m not blind” litany.
Ease of Passing: At times, “passing” as sighted is simply easier than delving into detailed explanations of personal limitations. This approach helps avoid the use of terms like “disabled” or “impaired,” which can steer conversations into uncomfortable or negative territory. Responding to such terms, listeners may exhibit patronizing attitudes or expressions of pity. To sidestep these reactions, visually impaired individuals may choose to pass as sighted for their own comfort and that of those around them.
Persistent Biases: Despite advancements in legislation and changing social attitudes toward disabilities, personal biases still linger, affecting how individuals perceive and react to disability. These lingering biases contribute to the inclination to conceal one’s visual impairment in social settings.
Self-Image: For those newly experiencing visual impairment, acceptance of their low vision may still be an ongoing journey. Choosing to remain silent about their disability can be a defense mechanism to uphold feelings of self-worth and a sense of “normalcy.”
Social Stigma and Self-Esteem: The societal stigma surrounding disabilities can lead to negative self-perceptions among the visually impaired. They may struggle with feelings of low self-esteem, perceiving themselves as “less-than” others.
Our self-perception is often influenced by how others perceive us. By not openly declaring “I am visually impaired,” individuals with disabilities aim to maintain equal standing with their peers. This is an attempt to resist being solely defined by their disability.
Privacy Concerns: Disclosing one’s disability and sharing personal details can feel invasive. Many visually impaired individuals view their visual status as private information, to be disclosed on a need-to-know basis.
Shame and Embarrassment: Past experiences with impaired vision that led to embarrassment or feelings of inferiority can result in a deep sense of shame. Others seem superior because they can see more quickly, react appropriately, and are queued into nuances of social interaction.
All of these seemingly small details of social interaction work due to better visual acuity. Facial recognition, facial expression, and visual jokes are missed by those with low vision leaving them to feel left out and embarrassed. Passing as sighted becomes a method of hiding what they perceive as a weakness or inadequacy.
Social Exclusion and Fear: Fear plays a significant role in this dynamic:
- Fear of loss of social acceptance.
- Fear of being marginalized or excluded and loss of social status.
- Fear of losing a job because of assumptions made by others who do not understand .
- Fear of Self-Realization: Admitting to oneself that they are not “normal” can be a daunting and fearful prospect.
- Fear of Social Judgment: The anxiety of having to explain their visual impairment in detail, knowing others will pass judgment.
- Fear of being singled out or treated differently due to their disability.
In navigating these complex emotions and societal pressures, visually impaired individuals often find themselves balancing between maintaining their privacy, preserving their self-image, and navigating a world that often fails to fully understand their experiences.
Also see this article on Why Those with Low Vision Have a Problem with Facial Recognition
How Children Learn to Pass
Pretending to See: Children often adjust their behavior to match what they believe others expect of them, sometimes pretending to see more or less than they actually can.
Parental Influence: Children are keen observers of their parents’ attitudes and fears. They quickly pick up on the concern surrounding their visual impairment, learning that not seeing what others see is viewed as a problem. To gain approval and avoid worry, children may give false responses, pretending to see things they actually can’t. The parent’s relief and positive reinforcement become a reward for their pretense.
Avoidance and Ignorance: Parents may sometimes choose to ignore the issue, perhaps due to difficulty in facing the reality of having a visually impaired child. This avoidance communicates to the child that their visual disability is something to be disregarded, contributing to their learning to “pass.”
Negative Attention in School: As school-age children, they quickly learn that being different can attract negative attention from peers. Other children may not always be kind or understanding, leading to feelings of exclusion and loneliness.
Treatment and Bullying: Disabled children may be treated as “special,” often being segregated from other children and excluded from certain activities due to accessibility challenges. They might also be infantilized, treated more childishly than their sighted peers. This difference in treatment can make them targets for bullying, which can be deeply upsetting and isolating.
Academic Impact: In attempting to pass as normal and avoid negative attention, children may also avoid asking for necessary help. This can result in falling behind academically, as their reluctance to seek assistance hampers their learning progress.
These experiences of social exclusion, bullying, and the pressure to conform to societal norms can have profound effects on a child’s development and self-esteem. As they navigate these challenges, children with visual disabilities often learn to hide their disability as a means of coping with the complexities of their social environment.
The consequences of pretending to be normal.
Social Awkwardness: When others are unaware of the limitations faced by someone concealing their visual impairment, the visually impaired individual may appear socially awkward. Due to their low vision, they might struggle to recognize faces, interpret facial expressions, and grasp nonverbal cues essential for social interaction. This can lead them to appear distracted or unresponsive in social situations.
Discomfort and Embarrassment: Admitting to not being able to see adequately after concealing it for some time can be uncomfortable and embarrassing. Those who were unaware may feel suspicious upon learning this information, wondering why it was kept hidden.
Navigating Social Situations: Navigating social situations with a visual impairment is inherently challenging. This challenge is compounded when others fail to understand the social mistakes that might occur, mistakes not typically made by those with normal vision. Consequently, visually impaired individuals may withdraw from social interactions, leading to feelings of depression and anxiety.
See my article on: Low Vision, Depression, and Anxiety
Employment Challenges: Concealing visual impairment from potential employers can pose significant challenges. Passing as sighted may seem like a way to bypass personal biases that some employers have against hiring disabled individuals. Despite legislation aimed at preventing discrimination, it unfortunately still exists.
Lack of Reasonable Accommodations: Failing to disclose vision loss to an employer means that necessary adjustments to accommodate low vision won’t be made. This can hinder the visually impaired individual from performing their job to the best of their ability. While some employers may be willing to make these adjustments, others may not understand or be open to the idea.
Risk of Errors and Job Loss: Attempting to pass as sighted comes with the risk of making unnecessary errors due to unmet visual needs. This could potentially result in losing a job for which reasonable accommodations could have been made.
Opportunity for Education and Awareness: Revealing one’s limitations is not just about personal acceptance; it’s also an opportunity to educate others. Just as the LGBTQ community has brought awareness and acceptance to their experiences, those with disabilities can also benefit from greater understanding. It’s crucial for others to realize that individuals with impairments are simply a different form of normal, deserving of respect, understanding, and the accommodations necessary to thrive.
In the end…..
Passing with a visual impairment presents numerous challenges, from social awkwardness to employment uncertainties. The decision to conceal one’s disability is often driven by social pressures and fear of stigma. However, there can be consequences leading to discomfort, social difficulties, and missed opportunities for accommodations.
Revealing one’s limitations can promote understanding and empathy, fostering a society that values inclusivity. By supporting individuals with visual impairments, we can create a world where everyone can thrive.
Read more about the Experience of Being Visually Disabled: How Vision Loss Affects the Social, Emotional, and Practical Aspects of Life